The Omicron variant of SARS-CoV-2 is spreading at an alarming rate. It could soon replace the Delta variant, which at present dominates globally. However, little is known about whether currently available vaccines and drugs will be effective against the Omicron variant. To assess the efficiency of vaccines and therapeutic antibodies, a research team led by Stefan Pöhlmann and Markus Hoffmann from the German Primate Center - Leibniz Institute for Primate Research in Göttingen and colleagues from the Hannover Medical School, the University of Göttingen Medical Center, the Friedrich-Alexander University of Erlangen-Nürnberg and the German Center for Infection Research in Braunschweig, have studied how efficiently the Omicron variant is neutralized by antibodies from recovered and vaccinated people. The team was able to show that antibodies from recovered persons hardly inhibit the Omicron variant. Antibodies after two BioNTech-Pfizer vaccinations also showed significantly reduced efficacy against the Omicron variant. Better inhibition was observed after triple BioNTech-Pfizer vaccination as well as after heterologous vaccination with Oxford-AstraZeneca and BioNTech-Pfizer. Finally, most of the therapeutic antibodies evaluated in the study were not effective against the Omicron variant. These results indicate that several antibodies used to treat COVID-19 will be ineffective against the Omicron variant. However, they also suggest that a third immunization with the BioNTech-Pfizer vaccine (booster) and heterologous immunization may protect well against the Omicron variant.
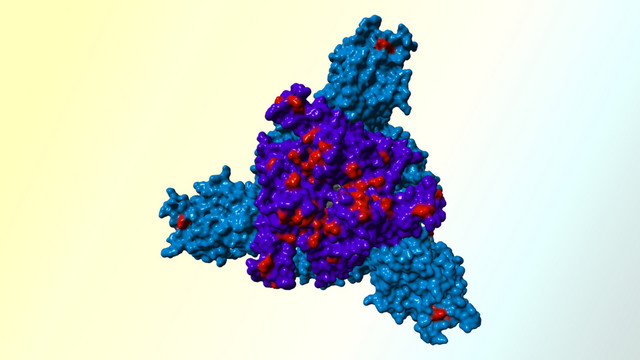
The Omicron variant of SARS-CoV-2 appears to be spreading faster than any previous variant and may soon dominate globally. Infection with SARS-CoV-2 and vaccination leads to the production of antibodies that strongly contribute to protection against severe disease. In addition, combinations of antibodies produced by biotechnology approaches are being used to treat COVID-19. The spike protein of SARS-CoV-2 facilitates viral entry into cells and constitutes the central target for antibodies that inhibit (neutralize) the virus. Therefore, it is important to determine whether the Omicron spike is inhibited by antibodies induced upon vaccination or infection or currently used for COVID-19 treatment. The researchers investigated these questions using non-hazardous virus-like particles that carry the Omicron spike and are well suited for analysis of virus entry and its inhibition.
Currently, combinations of the antibodies Casirivimab and Imdevimab, and Etesevimab and Bamlanivimab are used to treat COVID-19. However, the DPZ team showed that these antibodies are largely ineffective against the Omicron spike. Only one antibody, Sotrovimab, inhibited the Omicron spike. "Our cell culture studies suggest that most antibodies currently available for COVID-19 therapy will be ineffective against Omicron. Sotrovimab is an exception and could become an important treatment option for Omicron-infected patients," concluded first author Markus Hoffmann.
The researchers further investigated whether patients infected in Germany during the first wave of the pandemic had produced antibodies that protect against the Omicron variant. While the antibodies inhibited the spike of the virus responsible for the first wave, they had little effect against the Omicron spike. Therefore, it can be assumed that these individuals do not have robust immune protection against the Omicron variant, although an inhibition by T cells, which are also produced during infection, remains to be analyzed.
Antibodies produced after two immunizations with the BioNTech-Pfizer vaccine also inhibited the Omicron spike significantly less efficiently than the spike proteins of other variants. A better protective effect was observed after three immunizations with BioNTech-Pfizer and after heterologous immunization with Oxford-AstraZeneca/BioNTech-Pfizer. These results indicate that dual immunization with BioNTech-Pfizer may protect less efficiently against the Omicron variant as compared to the Delta variant. In contrast, triple immunization with BioNTech-Pfizer (booster) and cross-vaccination with Oxford-AstraZeneca/BioNTech-Pfizer could establish stronger protection.
"Our results indicate that antibody therapies for COVID-19 need to be adapted to the Omicron variant. Adaptation of the BioNTech-Pfizer vaccine should also be considered. In contrast, triple immunization with BioNTech-Pfizer (booster) and cross-vaccination with Oxford-AstraZeneca/BioNTech-Pfizer could provide protection against the Omicron variant," says Stefan Pöhlmann.
Original publication
Hoffmann, M., Krüger, N., Schulz, S., Cossmann, A., Rocha, C., Kempf, A., Nehlmeier, I., Graichen, L., Moldenhauer, A.-S., Winkler, M.S., Lier, M., Dopfer-Jablonka, A., Jäck, H.-M., Behrens, G.M.N., Pöhlmann, S., The Omicron variant is highly resistant against antibodymediated neutralization – implications for control of the COVID-19 pandemic, Cell (2022), doi: doi.org/10.1016/j.cell.2021.12.032.
Contact
Prof. Dr. Stefan Pöhlmann
+49 551 3851-150
Profile